ABC News – Feb 23, 2011
by Dr. Stefan Kruszewski, Psychiatrist and CEO of Kruszewski & Associates, a Pennsylvania based firm specializing in illuminating healthcare and financial fraud.
"In fact, no one in the medical industry is a bigger offender when it comes to mistreatment than those of us in psychiatry."
With a few exceptions, when physicians talk, they recommend. Take this. Try that. They satisfy the expectation that automatically comes with a patient’s visit or phone call. The physician is compelled to make a recommendation — a pill, a device or a procedure. Both the physician and medical supplier financially benefit. But is your doctor’s advice always in your best interest?
Not always.
In a 2000 JAMA publication, Julie Magno Zito of the University of Maryland and her coauthors stated that there had been an explosion in psychotropic prescriptions for pre-schoolers without adequate safety and long-term studies and generally without FDA approvals.
Dr. Joseph Coyle of Harvard Medical School editorialized on this “troubling change in practice.”
Likewise, in a 2001 JAMA article, Dr. Chunliu Zhan of the Agency for Healthcare Research and Quality and his colleagues found that American elderly patients are often overly and inappropriately medicated.
And, there are medical errors. Reports from the Institute of Medicine and HealthGrades indicate that there have been 400,000 to 1.2 million error-induced deaths in the United States from 1996 to 2006.
Excessive medications and procedures, adverse events and medical errors are endemic to medicine. In the early 1990s, surgeons were encouraged to perform quadruple bypass surgery for heart disease. Recent studies now suggest the surgery was, in many cases, a waste of time and money, improving neither morbidity nor mortality.
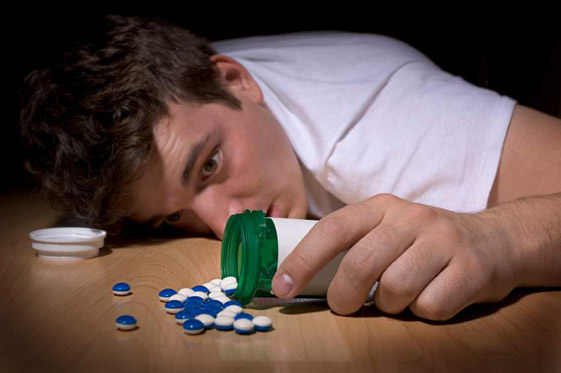
Surgeons are not the only medical professionals who misdiagnose and perform unnecessary procedures. In fact, no one in the medical industry is a bigger offender when it comes to mistreatment than those of us in psychiatry. With psychoactive diagnoses and medications, I’m currently seeing a trend among doctors prescribing adolescents with stimulants for bogus reports of ADD. In the most common occurrence, the doctor misses the diagnoses of daily marijuana abuse, alcohol abuse and oxycodone abuse.
Many doctors fail to perform a simple urine drug screen, treating instead the residual drug-related symptoms of inattention, lack of motivation, poor academic performance and forgetfulness with amphetamines, antidepressants or antipsychotics.
At worst, kids receive all three medications together, which is dangerous in immeasurable ways. This also happens to adults.
When ‘Medicine’ Makes Things Worse
In the past, psychiatric physicians have diagnosed homosexuality, paraphrenia, paranoia, narcissism, neuroses, combat fatigue and other entities, treating those “disorders” with a variety of therapies, including pills.
More recently, psychiatrists diagnose bipolar disorder not otherwise specified (NOS), adult attention deficit disorder and pre-psychotic conditions, for which they may prescribe pills. The problem is that some of those earlier diagnoses like (homosexuality, neuroses, combat fatigue, paranoia and paraphrenia) no longer exist as entities recognized by the DSM-IV-TR — the most current compendium of mental conditions and disorders.
Virtually anyone at any given time can meet the criteria for bipolar disorder NOS or ADD. Anyone. And the problem is everyone diagnosed with even one of these illnesses triggers the pill dispenser.
Taking stimulants, antidepressants, antipsychotics or off-label use of anti-convulsants often obscures the real problem and instead adds a new layer of unintended adverse events that only make conditions worse.
My advice to doctors: It’s OK not to prescribe anything. It’s OK to listen, to do no harm, to offer compassionate and helpful living advice. It can be therapeutic to recommend abstinence from cigarettes, drugs and alcohol, to eat more nutritiously, to sustain a relationship, lose weight, volunteer, meditate, pray, walk, laugh, sing, play music and embrace kindness.
It’s also OK to offer the patient a metaphorical motivational kick and advise them to just do something to help themselves. That may do more to improve outcomes and reduce adverse events and unnecessary prescribing than an injudiciously prescribed pill or procedure.
Many doctors fail to perform a simple urine drug screen, treating instead the residual drug-related symptoms of inattention, lack of motivation, poor academic performance and forgetfulness with amphetamines, antidepressants or antipsychotics.
At worst, kids receive all three medications together, which is dangerous in immeasurable ways. This also happens to adults.
http://abcnews.go.com/Health/Wellness/prescribing-improve-outcomes/story?id=12973777


SHARE YOUR STORY/COMMENT