
Top psychiatrist: ‘We are turning childhood into a disease’
Amy Bevis wasn’t schizophrenic – she was being bullied at school.


Amy Bevis wasn’t schizophrenic – she was being bullied at school.

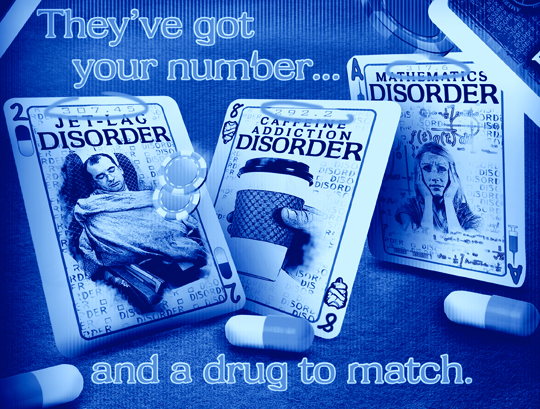
More and more people around you are being diagnosed with depression or ADHD, but is that an illusion?

As if mental health patients are not already taking enough pharmaceuticals, a group of scientists from the U.K. recently published a study chastising the mental health profession for allegedly “under-medicating” those with mental illnesses. According to the outrageous study, which was published in the British Journal of Psychiatry, the physical health needs of mental patients are apparently being overlooked, which is causing many of these patients to suffer cardiovascular disease and various other conditions at a measurably higher rate than the rest of the population.

Every decade or two, the American Psychiatric Association reworks its Diagnostic Statistical Manual, or DSM, to try to have diagnostic categories reflect the current state of theory and practice. Given enormous evidence that we’re currently overdiagnosing things and medicalizing normal behavior, many had hope that the upcoming DMS-5 — the fifth major revision — would show some restraint. We may see it yet — but not if we go down the track described in a post today by neuroscientist, blogger, and DSM watchdog Neuroskeptic:. It seems that the DSM-5 may include a new proposed “mood disorder” called “disruptive mood dysregulation disorder,” or DMDD.
YOU’VE got to feel sorry for the American Psychiatric Association, at least for a moment. Its members proposed a change to the definition of autism in the fifth edition of their Diagnostic and Statistical Manual of Mental Disorders, one that would eliminate the separate category of Asperger syndrome in 2013. And the next thing they knew, a prominent psychiatrist was quoted in a front-page article in this paper saying the result would be fewer diagnoses, which would mean fewer troubled children eligible for services like special education and disability payments.
Then, just a few days later, another front-pager featured a pair of equally prominent experts explaining their smackdown of the A.P.A.’s proposal to eliminate the “bereavement exclusion” — the two months granted the grieving before their mourning can be classified as “major” depression. This time, the problem was that the move would raise the numbers of people with the diagnosis, increasing health care costs and the use of already pervasive mind-altering drugs, as well as pathologizing a normal life experience.
Fewer patients, more patients: the A.P.A. just can’t win. Someone is always mad at it for its diagnostic manual.