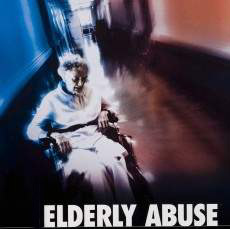
Use of chemical restraints in nursing homes called an epidemic
Nearly 25 percent of the residents in California’s nursing homes are placed on antipsychotic drugs, often used as sort of a chemical leash to control behavior in a trend a watchdog called an epidemic Thursday at a symposium. The drugs can double the risk of death for seniors with dementia and cause side effects ranging from stroke to delirium, according to speakers at an Oxnard conference called “Toxic Medicine.”