By Jan Eastgate
President, CCHR International
The Mental Health Industry Watchdog
August 5, 2019
Global antidepressant use is soaring, putting millions at risk of suicide, including in teens, while studies also show the drugs to be “largely ineffective and potentially harmful.”[1] The U.S. National Institute of Mental Health (NIMH) reports that as many as two-thirds of those taking antidepressants do not recover from depression,[2] but fail to warn that the drugs can drive consumers to suicide and violence. The drugs are also addictive and could cause intracranial hemorrhage and other physically damaging effects.
While there may be numerous reasons for the spate of mass murders and violent crime we see today, the fact remains that psychiatric drugs play a role in many acts of mass violence, which requires government investigation. Drug regulatory agencies around the world have issued 27 warnings of violence, aggression, hostility, mania, psychosis or homicidal ideation linked to psychotropic drugs and nearly 50 warnings about self-harm or suicide/suicidal ideation.[3] Add to that, leading medical and psychiatric journals have published studies and research findings supporting these warnings, at least 12 of which are about antidepressants.
Between 2000 and 2015, antidepressant prescriptions increased in all 29 countries surveyed by the Organization for Economic Co-operation and Development, on average doubling.[4] The U.S. ranks among the highest with 43 million Americans currently taking antidepressants.[5]
Shockingly, IQVia’s statistics for 2017 show that more than 2.1 million 0-17 year olds in the U.S. are prescribed antidepressants despite the 2004 Food and Drug Administration (FDA) Black Box warning that the drugs may cause suicide. Even more worrying is that of these, 38,534 are aged 0-5 and 574,090 are 6-12 years old.[6] As a nation, that should be of considerable concern.
According to the National Center for Health Statistics (NCHS), the rate of antidepressant use among teens and adults increased by almost 400% between 1988–1994 and 2005–2008.[7] And this is seen as a source of increasing suicides.
- In 2017, Martin Plöderl, Ph.D. and Michael P. Hengartner, PD. reported findings from research and stated: “if you look at the past 10 years, antidepressant rates are associated with increased suicide rates,” the drugs “most likely cause suicidal behavior in young people” and “data strongly suggest that antidepressants can cause suicides and aggressive behavior.”[8]
- A study from the Nordic Cochrane Centre and the University of Copenhagen published in the peer-reviewed British Medical Journal (BMJ) in 2016 also concluded that “children and young people are more likely to think about or attempt suicide while taking antidepressants.”[9]
UN Calls for Changes to “Biomedical” Mental Health Model
There are global concerns about a growing dependency upon a biological approach to treating mental health issues. In 2017, the United Nations Special Rapporteur on the right to health, Dainius Pūras, reported: “There is now unequivocal evidence of the failures of a system that relies too heavily on the biomedical model of mental health services, including the front-line and excessive use of psychotropic medicines, and yet these models persist.” Mr. Pūras warned that power and decision-making in mental health are concentrated in the hands of “biomedical gatekeepers,” particularly those representing biological psychiatry and called for a sea of change in mental health care around the world.[10]
In an interview for CNN in 2007, Dr. Ronald Dworkin, one of many critics who believe too many doctors unnecessarily prescribe antidepressants, said: “Doctors are now medicating unhappiness. Too many people take drugs when they really need to be making changes in their lives.”[11]
Theodore Dalrymple, writing in Spectator USA, also stated: “Unhappiness is far too often diagnosed as depression – and treated as such” and “It is as if the word unhappy had disappeared from the lexicon altogether and happiness were the normal condition of mankind, deviation from which were pathological.”[12]
It’s not saying that people that are in need of emotional help, shouldn’t get it, but information they get is skewed in an industry that profits billions of dollars from people being told to medicate their problems with antidepressants and other psychotropic drugs. Today, around 40 antidepressants are on the market and are among the most commonly prescribed drugs in many Western countries.[13] With it, we see increasing acts of senseless violence and suicide—adverse effects clearly linked to the drugs.
CCHR: What It Believes
Watch video: CCHR—What We Believe
The Citizens Commission on Human Rights (CCHR) recognizes that mental travail and despair exist. But these are not “diseases,” as there is no evidence of physical/medical abnormality for any psychiatric disorder or a medical test to confirm it. The failure to make this clear to consumers, including the myth that a “chemical imbalance” is causing their depression to reinforce the need to take an antidepressant, is arguably consumer fraud.
CCHR’s co-founder, the late Dr. Thomas Szasz, professor of psychiatry, pointed out: “There are no objective diagnostic tests to confirm or disconfirm the diagnosis of depression; the diagnosis can and must be made solely on the basis of the patient’s appearance and behavior and the reports of others about his behavior.”[14]
Even Thomas Insel, psychiatrist, and former Director of the National Institute for Mental Health (NIMH), concurs, saying, psychiatric “diagnoses are based on a consensus [vote] about clusters of clinical symptoms, not any objective laboratory measure [tests].”[15]
Matt Rudorfer, a psychiatrist and program chief of the division of services and intervention research at NIMH also concedes: “When we have a treatment that shows effect, we infer what it’s doing in the brain, but we really don’t know.”[16]
People choosing to take an antidepressant are rarely, if ever, informed of such information. In discussing one study, the lead author, Tony Z. Tang, Ph.D., a professor of psychology at Northwestern University in Evanston, Illinois said: “Medication can definitely change people’s personalities, and change them quite substantially,” but that can mean a “tendency toward emotional instability and negative mood.”[17]
An antidepressant may give a feeling of “relief” but that’s the trap. So does alcohol, cocaine or any mind-altering drug. Getting off them can be extremely difficult and for years psychiatrists and doctors have told patients that the debilitating effects they experience withdrawing from antidepressants or other psychotropics are their “illness” returning and not the iatrogenic induced adverse condition.
It’s a point that psychiatrist Allen Frances made in an interview with CNN on May 16, 2018, called “How Antidepressant Withdrawal ‘Can Trap People.’” Frances said, “There’s absolutely no interest on the part of the pharmaceutical companies in advertising the fact that getting on an antidepressant may trap you for years and maybe for life….”[18]
Furthermore, untreated medical conditions can manifest as “mental disorder.”
In the 1980s, CCHR had helped obtain a pilot study on the failure of psychiatrists to properly diagnose medical conditions in nearly 40% of patients admitted to a California state psychiatric hospital. According to the California Department of Mental Health Medical Evaluation Field Manual that ensued from this study, mental health professionals “have a professional and a legal observation to recognize the presence of physical disease in their patients….”[19]
But as Dr. Mary Anne Block D.O., author of Just Because You’re Depressed Doesn’t Mean You Have Depression: Depression is a Symptom Not a Disease, says, many psychiatrists do not conduct physical examinations before prescribing drugs.[20]
 CCHR works with medical doctors and in a booklet specifically written for physicians, it states: “It has long been the policy of CCHR that anyone with a physical or mental condition should first see a competent, non-psychiatric physician to ensure an undiagnosed, untreated physical condition is not causing ‘psychiatric’ symptoms. While CCHR does not, itself, give medical advice, we advocate standard medical care.”
CCHR works with medical doctors and in a booklet specifically written for physicians, it states: “It has long been the policy of CCHR that anyone with a physical or mental condition should first see a competent, non-psychiatric physician to ensure an undiagnosed, untreated physical condition is not causing ‘psychiatric’ symptoms. While CCHR does not, itself, give medical advice, we advocate standard medical care.”
But these days, general practitioners prescribe the majority of antidepressants and are contributing to the violent chaos these drugs can produce.
Dismissing important facts about antidepressants that have been reported in peer-review medical journals and by the FDA and other drug regulatory agencies does a tremendous disservice to consumers and puts them at risk, for which their prescribers should be held accountable.
The bottom line is a $4.6 billion a year antidepressant market is being put before patients’ safety and welfare. In the U.S., one of only two countries that allow Direct to Consumer (DTC) marketing, prescription drug advertising increased from $1.3 billion (79,000 ads) to $6 billion (4.6 million ads [including 663,000 TV commercials]) between 1997 and 2016.[21] Antidepressants were among the top advertised Rx category in 2010 and $643 million was spent on advertising mental health drugs.[22]
In 2015, the American Medical Association called for a ban on DTC advertising of prescription drugs to consumers.[23]
Networks—ABC, CBS, NBC—along with cable channels like CNN draw a lot of the pharmaceutical advertising. According to Jon Swallen, chief research officer at Kantar Media, a consulting firm that tracks multimedia advertising, the effect of the ban on networks would be a daunting, 8% loss of total ad revenue.[24]
Get all the Facts—Not Just Those Touted by Vested Interests
The bottom line with SSRI antidepressants is that there are far more risks, including withdrawal effects, that consumers were not informed of when the drugs first came on the market. And manufacturers and prescribing psychiatrists and doctors have profited from it.
Allan Horwitz, Ph.D., in a review published in The Medscape Journal in 2008, wrote: “After a rapturous reception [given SSRIs] upon their introduction in the late 1980s, which persisted until the emergence of uncertainty during the early years of the 21st century, we are now witnessing a rising chorus of cynicism and disbelief about these drugs. [Lecturer in psychiatry at Yale Medical School] Charles Barber’s Comfortably Numb joins the increasingly long list of books that are written for a general audience and question the widespread use of SSRIs.”[25]
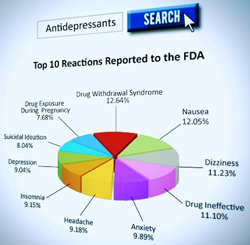 CCHR provides resources for consumers. It’s online Psychiatric Drugs Side Effects Database includes decrypted FDA adverse drug reports which can be easily searched online.
CCHR provides resources for consumers. It’s online Psychiatric Drugs Side Effects Database includes decrypted FDA adverse drug reports which can be easily searched online.
CCHR supports the United Nations Special Rapporteur Dainius Pūras’ advice that “It is crucial now to assess the root causes of failure and to chart a way forward, reaching consensus on the best way to do this.”[26] That failure includes the widespread use of psychotropic drugs that are not only harming individuals but also our communities and nations with increased suicides and acts of violence. To chart a way forward, there must be accountability and penalties for those manufacturers and prescribers of these dangerous chemicals where they result in damage, addiction, suicide and violence acts. Furthermore, drug regulatory agencies should be withdrawing such drugs from the market when they are endangering lives.
Appendix: Antidepressants—A Quick Review
Ineffective & Relapse
A few examples of studies that consumers may not be aware of:
- A 2017 study published in Frontiers in Psychiatry concluded that “antidepressants are largely ineffective and potentially harmful.” Lead researcher Michael P. Hengartner at the Zurich University of Applied Sciences in Switzerland conducted a thorough literature review focusing on randomized, controlled trials — the gold standard of evidence-based recommendation. Hengartner cited evidence that the likelihood of relapse is also correlated with duration of treatment. That is, the more one takes an antidepressant, the likelier one is to have another episode of depression.[27]
- In the well-publicized NIMH STAR*D study, which followed nearly 3,000 antidepressant users, only one-third went into remission after several months. Many of the rest moved on to a different drug, but in total, after trying as many as four separate drugs and combinations, fully 33% remained symptomatic. [28]
- On 16 May 2016, the Medical Journal of Australia reported, “The use of antidepressants has continued to rise despite accumulating evidence that they are not as effective as was previously thought.”[29]
- In addition to the usual serious adverse effects of antidepressants, a JAMA Neurology study in 2017 found the use of SSRIs and more generally of antidepressants that are strong inhibitors of serotonin reuptake were associated with an increased risk for intracranial hemorrhage compared with tricyclic antidepressants, particularly in the first 30 days of use.[30]
- TIME reported in 2016 that the studies “don’t support a strong effectiveness of antidepressants among kids should give doctors pause when considering a first-line treatment.” [31]
Antidepressants Cause Suicides
- A 2016 review of clinical trial data published by the Royal Society of Medicine determined the suicide risk from antidepressants is also evident in those older than 24, stating: “antidepressants double the occurrence of events in adult healthy volunteers that can lead to suicide and violence.[32]
- The UK National Health Services (NHS) reported in 2016 that “researchers analyzed 70 studies which looked at five antidepressants. They looked specifically at the reports of deaths, suicides, suicidal thinking or suicide attempts, aggression, and a type of extreme restlessness called akathisia. The results showed that children taking antidepressants had a higher chance of suicidal thoughts or suicide attempts, and of aggression.”[33]
- Children and young adults who started taking SSRI antidepressants in higher-than-average doses were also twice as likely to attempt suicide as people taking average doses, according to a study published in JAMA Internal Medicine. [34]
- In 2018, Plöderl and Hengartner reported findings from their research, which includes that from 2000 onwards, suicide rates in the U.S. started to rise among youth around 2007, despite the FDA Black Box warning in 2004 that antidepressants are linked to suicide in those aged 18 and younger. They pointed out that “antidepressant prescription rates steadily increased” until today and added: “mainstream psychiatry will continue to claim that antidepressants effectively reduce suicide risk, despite compelling evidence to the contrary.” They go further to say there is “increasing certainty that antidepressants are rather ineffective and most likely cause suicidal behavior in young people….”[35] The suicide rate among Americans ages 35 to 64 rose by roughly 28% between 1999 and 2010, according to a Centers for Disease Control and Prevention.[36] Simultaneously, there was a 64% increase in the percentage of people using antidepressants between 1999 and 2014.”[37]
- As further confirmation, in 2016, NPR reported that in the ’80s and ’90s, America’s suicide trend was headed in the right direction: down. “It had been decreasing almost steadily since 1986, and then what happened is there was a turnaround,” said Sally Curtin, a statistician with the NCHS, part of the Centers for Disease Control and Prevention. Girls between the ages of 10 and 14, while making up a very small portion of the total suicides, experienced the largest percent increase, tripling over 15 years from 0.5 to 1.7 per 100,000 people.[38]
- Kelly O’Meara, author, journalist and former Congressional staffer, wrote a public awareness piece in 2014 about actor Robin Williams having been on antidepressants at the time of his suicide. The particular antidepressant, mirtazapine, (also known as Remeron) carries 10 international drug regulatory agency warnings on causing suicidal ideation. [39]
Antidepressant Withdrawal Effects
- In May 2019, the Royal College of Psychiatrists conceded the damaging withdrawal effects of antidepressants—that ending treatment can cause “severe” adverse effects and last much longer than previously advised—for weeks and even months.[40]
- In an article on antidepressant withdrawal for The New York Times, Benedict Carey reported that doctors for years “have dismissed or downplayed such symptoms, often attributing them to the recurrence of underlying mood problems.” Drug-makers also help minimize the problem by urging staff and publicists in internal memos, “Highlight the benign nature of discontinuation symptoms, rather than quibble about their incidence.”[41]
- In March 2019, Lancet Psychiatry published a study by University College London psychiatry researchers Mark Horowitz and David Taylor, arguing that responsible tapering of antidepressants should extend to months or even years, depending on the individual, not conclude in four weeks.[42]
- Post-withdrawal symptoms from antidepressants “may last several months to years” and include disturbed mood, emotional lability [excessive emotional reactions and frequent mood changes] and irritability, according to a study in Psychotherapy and Psychosomatics in 2012.[43]
- British psychiatrist Joanna Moncrieff and others reported in The Journal of Psychoactive Drugs, “It is now accepted that all major classes of psychiatric medication produce distinctive withdrawal effects which mostly reflect their pharmacological activity.”[44]
Women Targeted for Antidepressants
- Women constitute two-thirds of those given brain-damaging electroshock treatment and they’re also overrepresented for antidepressants. A 2017 JAMA study found nearly one in six American women, some 16%, were on an antidepressant—three times more likely than their male peers to be taking one—some 9% vs. 3%.[45]
- Julie Holland, a psychiatrist in private practice in New York, believes doctors shouldn’t be so quick to label a woman’s volatile moods as abnormal. Holland especially fears that antidepressants blunt women’s full emotional range. “You lose the low end on these medications, but you also lose the high end: There’s less joy, creativity, empathy, and surprise,” she says.[46]
Antidepressants Create Violent Behavior
- Violent behavior is also a known side effect of antidepressants. A 2015 Swedish study of their entire population ages 15 and older reported that 11,225 out of 856,493 (1.3%) teens and adults taking SSRIs were convicted of a violent crime compared to 40,384 out of 7.1 million individuals (0.6%) of the same age not taking SSRIs. 3.3% of SSRI patients between the ages of 15 and 24 years old were convicted of a violent crime. 77% of these convictions (2,16
 9) were in males in that age group who were taking an SSRI. [47]
9) were in males in that age group who were taking an SSRI. [47]
CCHR produced a comprehensive report on Psychiatric Drugs Create Violence and Suicide, which provides studies and expert quotes about the potential link between prescription psychotropic drugs and a percent of violence, including mass shootings.
References:
[1] Michael P. Hengartner, “Methodological Flaws, Conflicts of Interest, and Scientific Fallacies: Implications for the Evaluation of Antidepressants’ Efficacy and Harm,” Frontiers in Psychiatry, 7 Dec. 2017, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5725408/
[2] “Doctors Are Too Quick to Give Women Antidepressants,” Vice, 27 Jun. 2017, citing: https://www.vice.com/en_us/article/43yjbj/doctors-are-too-quick-to-give-women-antidepressants.
[3] https://www.cchrint.org/pdfs/violence-report.pdf, p. 3.
[4] “Nobody can agree about antidepressants. Here’s what you need to know,” New Scientist, 2 Oct. 2018, https://www.newscientist.com/article/mg23931980-100-nobody-can-agree-about-antidepressants-heres-what-you-need-to-know/.
[5] IQVia Total Patient Tracker (TPT) Database, Year 2017, Extracted April 2018.
[6] https://www.cchrint.org/psychiatric-drugs/children-on-psychiatric-drugs/.
[7] “Astounding increase in antidepressant use by Americans,” Harvard Health Publishing, 20 Oct. 2011, https://www.health.harvard.edu/blog/astounding-increase-in-antidepressant-use-by-americans-201110203624; “Antidepressants: Top Advertised & 3rd Most Commonly Used Rx Drug,” Pharma Marketing Blog, 24 Oct. 2011, http://pharmamkting.blogspot.com/2011/10/antidepressants-top-advertised-3rd-most.html.
[8] Martin Plöderl, PhD & Michael P. Hengartner, Ph.D., “Suicides Are Increasing – And So Are Antidepressant Prescriptions,” MAD, 23 Aug. 2018, https://www.madinamerica.com/2018/08/suicides-are-increasing-and-so-are-antidepressant-prescriptions/.
[9] “Antidepressants linked to suicide and aggression in teens,” NHS (UK), 28 Jan. 2016, https://www.nhs.uk/news/mental-health/antidepressants-linked-to-suicide-and-aggression-in-teens/.
[10]“World needs “revolution” in mental health care – UN rights expert,” United Nations Human Rights Officer of the High Commissioner, 6 June 2017, https://www.ohchr.org/EN/NewsEvents/Pages/DisplayNews.aspx?NewsID=21689.
[11] https://www.addictioncenter.com/stimulants/antidepressants/symptoms-signs/.
[12] Theodore Dalrymple, “Why Marianne Williamson is right about antidepressants,” Spectator USA, 1 Aug. 2019, https://spectator.us/marianne-williamson-right-antidepressants/.
[13] “Nobody can agree about antidepressants. Here’s what you need to know,” New Scientist, 2 Oct. 2018, https://www.newscientist.com/article/mg23931980-100-nobody-can-agree-about-antidepressants-heres-what-you-need-to-know/.
[14] https://www.cchrint.org/about-us/co-founder-dr-thomas-szasz/.
[15] Thomas Insel, “Transforming Diagnosis,” NIMH Website, 20 Apr. 2013, http://www.nimh.nih.gov/about/director/2013/transforming-diagnosis.shtml.
[16] “Doctors Are Too Quick to Give Women Antidepressants,” Vice, 27 Jun. 2017, citing: https://www.vice.com/en_us/article/43yjbj/doctors-are-too-quick-to-give-women-antidepressants.
[17] Anne Harding, “Antidepressants change personality, study suggests,” 8 Dec. 2009, http://www.cnn.com/2009/HEALTH/12/08/antidepressant.personality.changes/index.html.
[18] https://www.madinamerica.com/2018/10/allen-frances-increasing-use-antidepressants/.
[19] Lorrin M. Koran, M.D., Department of Psychiatry and Behavioral Sciences, MEDICAL EVALUATION FIELD MANUAL, Standford, CA, 1991, https://www.alternativementalhealth.com/medical-evaluation-field-manual/.
[20] Mary Ann Block, DO, Just Because Your Depressed Doesn’t Mean You Have Depression, Or Depression Is a Symptom Not a Disease So Find the Cause Fix the Problem, (The Block System, 2007), pp. 21-26.
[21] “Medical Marketing in the United States, 1997-2016,” JAMA, 1/8 Jan. 2019, https://jamanetwork.com/journals/jama/fullarticle/2720029.
[22] “Antidepressants: Top Advertised & 3rd Most Commonly Used Rx Drug,” Pharma Marketing Blog, 24 Oct. 2011, http://pharmamarketing.blogspot.com/2011/10/antidepressants-top-advertised-3rd-most.html; https://www.tandfonline.com/doi/abs/10.1080/02650487.2014.994802?scroll=top&needAccess=true&journalCode=rina20.
[23] Ed Silverman, “American Medical Association wants to ban drug ads to consumers,” STAT, 17 Nov. 2015, https://www.statnews.com/pharmalot/2015/11/17/pharmalot-ama-drugs/.
[24] Bruce Horovitz and Julie Appleby, “Prescription drug costs are up; So are TV ads promoting them,” Kaiser Health News, printed USA Today, 16 Mar. 2017, https://www.usatoday.com/story/money/2017/03/16/prescription-drug-costs-up-tv-ads/99203878/.
[25] “Comfortably Numb: How Psychiatry Is Medicating a Nation,” Medscape J Med. 2008; 10(5): 121, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2438484/.
[26] “World needs “revolution” in mental health care – UN rights expert,” United Nations Human Rights Officer of the High Commissioner, 6 June 2017, https://www.ohchr.org/EN/NewsEvents/Pages/DisplayNews.aspx?NewsID=21689.
[27] Michael P. Hengartner, “Methodological Flaws, Conflicts of Interest, and Scientific Fallacies: Implications for the Evaluation of Antidepressants’ Efficacy and Harm,” Frontiers in Psychiatry, 7 Dec. 2017, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5725408/.
[28] “Doctors Are Too Quick to Give Women Antidepressants,” Vice, 27 Jun. 2017, citing: https://www.vice.com/en_us/article/43yjbj/doctors-are-too-quick-to-give-women-antidepressants.
[29] Christopher G Davey and Andrew M Chanen, “The unfulfilled promise of the antidepressant medications,” Med J Aust 2016; 204 (9): 348-350, https://www.mja.com.au/journal/2016/204/9/unfulfilled-promise-antidepressant-medications.
[30] Christel Renoux, MD, PhD et al., “Association of Selective Serotonin Reuptake Inhibitors With the Risk for Spontaneous Intracranial Hemorrhage,” JAMA Neurol. 2017;74(2):173-180. doi:10.1001/jamaneurol.2016.4529 , https://jamanetwork.com/journals/jamaneurology/article-abstract/2588683.
[31] “Teen Depression Treatment Is an Increasingly Thorny Issue,” TIME, 8 Jun. 2016, https://time.com/4361897/teen-depression-treatment-antidepressants/.
[32] Andreas Ø Bielefeldt, et al., “Precursors to suicidality and violence on antidepressants: systematic review of trials in adult healthy volunteers,” Journal of the Royal Society of Medicine, October 2016, Vol. 109, No. 10, p. 381, http://jrs.sagepub.com/content/109/10/381.full.
[33] “Antidepressants linked to suicide and aggression in teens,” NHS (UK), 28 Jan. 2016, https://www.nhs.uk/news/mental-health/antidepressants-linked-to-suicide-and-aggression-in-teens/.
[34] Nancy Shute, “Higher Doses Of Antidepressants May Raise Teen Suicide Risk,” NPR, 28 Apr. 2014, https://www.npr.org/sections/health-shots/2014/04/28/307671897/higher-doses-of-antidepressants-may-raise-teen-suicide-risk.
[35] Martin Plöderl, PhD & Michael P. Hengartner, Ph.D., “Suicides Are Increasing – And So Are Antidepressant Prescriptions,” MIA, 23 Aug. 2018, https://www.madinamerica.com/2018/08/suicides-are-increasing-and-so-are-antidepressant-prescriptions/.
[36] https://foreignpolicy.com/2013/05/03/how-does-americas-suicide-rate-compare-globally/.
[37] https://www.apa.org/monitor/2017/11/numbers.
[38] “Suicide Rates Climb In U.S., Especially Among Adolescent Girls,” NPR, 22 Apr. 2016, https://www.npr.org/sections/health-shots/2016/04/22/474888854/suicide-rates-climb-in-u-s-especially-among-adolescent-girls.
[39] https://www.globalresearch.ca/robin-williams-was-on-drugs-at-the-time-of-his-death-antidepressant-drugs/5413827.
[40] Christopher Lane, Ph.D., “Antidepressant Guidelines to Tighten in the UK: Welcome policy change also reveals scale of the problem,” Psychology Today, 31 May, 2019, https://www.psychologytoday.com/us/blog/side-effects/201905/antidepressant-guidelines-tighten-in-the-uk.
[41] Ibid.
[42] Ibid.
[43] “Patient Online Report of Selective Serotonin Reuptake Inhibitor-Induced Persistent Post-withdrawal Anxiety and Mood Disorders,” Psychotherapy and Psychosomatics, 19 Jan. 2012, https://www.karger.com/Article/FullText/341178.
[44] Joanna Moncrieff, M.B.B.S., et al., “The Psychoactive Effects of Psychiatric Medication: The Elephant in the Room,” Journal of Psychoactive Drugs, 45 (5), 409–415, 2013, https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4118946/.
[45] “Doctors Are Too Quick to Give Women Antidepressants,” Vice, 27 Jun. 2017, citing: https://www.vice.com/en_us/article/43yjbj/doctors-are-too-quick-to-give-women-antidepressants, citing “Adult Utilization of Psychiatric Drugs and Differences by Sex, Age, and Race,” JAMA Intern Med. 2017 Feb 1; 177(2):274-275. doi: 10.1001/jamainternmed.2016.7507, https://www.ncbi.nlm.nih.gov/pubmed/27942726.
[46] Ibid.
[47] http://www.center4research.org/antidepressants-increase-suicide-attempts-risks/ citing, Molero Y, Lichtenstein P, et al. Selective Serotonin Reuptake Inhibitors and Violent Crime: A Cohort Study. PLoS Med 12(9): e1001875. doi:10.1371/ journal.pmed.1001875.



SHARE YOUR STORY/COMMENT