The New American – March 17, 2014
By Rebecca Terrell
Dateline: Ontario, Canada. Eighteen-year-old Brennan McCartney visited his doctor for a chest cold and, despite no history of mental health issues or diagnosis of depression, received a prescription for the antidepressant Cipralex [also known as Lexapro]. Four days later, on November 8, 2010, he hanged himself.
Dateline: Laytonsville, Maryland. A psychiatrist prescribed the antidepressant Zoloft to 12-year-old Candace Downing, who suffered anxiety related to schoolwork but was otherwise a bright child with a loving family, a wide circle of friends, and no history of depression. On January 10, 2004, her mother found her dead, hanging from her bed valance.
Dateline: Indianapolis, Indiana. To help pay her college tuition, 19-year-old Traci Johnson volunteered for a clinical trial of a new antidepressant called Cymbalta. On February 7, 2004, she hanged herself at the Eli Lilly laboratory where the experiment was held. She was one of five participants who took their lives during clinical trials of the drug prior to its debut, though all had been pre-screened to confirm they did not have mental problems.
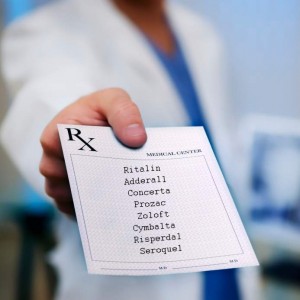
Thousands of similar stories link suicide, self-harm, and violent behavior to psychotherapeutics, but these medicines, often referred to as blockbuster drugs because they top $1 billion in annual sales, are among the most popular in medical history. The antipsychotic Abilify is now the nation’s top-selling drug. Research firm IMS Health reports sales totaled nearly $6.5 billion in 2013. The medicine involved in the clinical trial suicides recounted above, Cymbalta, is the fourth-most-prescribed drug in the United States and the fifth top seller at $5.2 billion. Vyvanse, an amphetamine used to treat childhood attention deficit hyperactivity disorder (ADHD), holds the eighth position on the list of most prescribed meds. Ninth is Lyrica, an anticonvulsant often used to treat social anxiety disorder. Number 36 is antipsychotic Seroquel, prescribed for a wide range of conditions from depression and anxiety to schizophrenia. Antidepressants are the most commonly prescribed medication class in the United States.
These cash cows can instigate mental conditions, such as suicidal ideation (preoccupation with suicide) and aggression. According to the Physician’s Desk Reference, an authoritative guide to prescription drug information, they can also cause serious physical side effects, especially involving the cardiovascular and central nervous systems. Psychotropics, as they are commonly called, include medicines to treat depression, anxiety, sleep disorders, and various psychoses, as well as stimulants used to treat attention deficit hyperactivity disorder. Antidepressants are particularly associated with high suicide risk, though most psychotropics carry suicide precautions, and all warn users to watch for increased depression and/or aggression. ADHD drugs are strongly linked with substance abuse, stunted growth, and even sudden death. Research shows long-term effects of psychotherapeutic medications pose other dangers. [See also Another Mass Shooting, Another Psychiatric Drug? Federal Investigation Long Overdue for more information on psychiatric drugs causing violent and suicidal behavior.]
Yet in a country where, according to the Centers for Disease Control and Prevention (CDC), heart disease, cancer, and chronic respiratory diseases claim the most lives, and Alzheimer’s disease and diabetes run rampant, there is a striking disconnect in the fact that four of the top 10 most-prescribed drugs are psychotropics. Why the soaring popularity of such dangerous substances?
To Drug or Not to Drug
 Practitioners believe benefits outweigh risks, pointing to the supposedly large number of people who profit from treatment and the fact that mental health problems and suicide are closely related. They argue that risk accompanies all medical treatments. But when the U.S. Food and Drug Administration (FDA) began requiring antidepressant manufacturers to label their products with a black box warning — the strongest measure short of pulling a drug from the market — alerting patients to the high risk of suicide, hostility, and agitation, key opinion leaders in the healthcare industry waged a media counterattack. They denied the problem and asserted the black box label added to adolescent suicide risk.
Practitioners believe benefits outweigh risks, pointing to the supposedly large number of people who profit from treatment and the fact that mental health problems and suicide are closely related. They argue that risk accompanies all medical treatments. But when the U.S. Food and Drug Administration (FDA) began requiring antidepressant manufacturers to label their products with a black box warning — the strongest measure short of pulling a drug from the market — alerting patients to the high risk of suicide, hostility, and agitation, key opinion leaders in the healthcare industry waged a media counterattack. They denied the problem and asserted the black box label added to adolescent suicide risk.
Shortly after the FDA issued its warning in 2004, Harvard Medical School published a newsletter claiming the agency had, “after much hesitation,” caved to “pressure from parents and Congress.” It credited antidepressants for a 15-percent decline in the U.S. adolescent suicide rate between 1985 and 1999 since those years saw an increase of nearly 70 percent in antidepressant use. We’ll see later that conflicts of interest within the FDA did indeed account for “much hesitation” prior to its issuing the warning. However, Harvard admitted clinical trials of antidepressants all showed “a consistent trend”: Compared with a placebo, antidepressants double the risk of suicidal thinking in both children and adults.
Critics of the FDA warning complain it has discouraged use of the black-boxed drugs in patients who would benefit from them. Appearing on National Public Radio in 2007, Dr. Ileana Arias, then head of the CDC Injury Division, indicated the warning was to blame for a rise in suicides. “We found that combined suicide rates for persons 10 to 24 years declined 28.5 percent from 1990 to 2003,” she observed. “But from 2003 to 2004, the rate increased by 8 percent, the largest single rise in 15 years.” Interestingly, CDC statistics reveal the suicide rate for that age group in 2007 (when Arias suggested the connection) was slightly less than it was in 2003. In fact, the rate was higher in 2010 than in any year of the previous decade, despite a CDC-reported increase in psychiatric medication use among adolescents between 2005 and 2010.
Today, one in 10 Americans takes at least one psychotropic, while suicide ranks as the tenth leading cause of death in the United States, the same ranking it held in 1980 before widespread use of antidepressants. Regrettably, the meds have not downgraded that rank, nor has the black-box warning damaged psychotropics’ popularity.
Marketing and Advertising
That’s no mystery, considering how diligently the drugs are promoted. Research published in the January 2008 edition of PLoS Med, a peer-reviewed medical journal, revealed the pharmaceutical industry spends almost twice as much on marketing as it does on research and development. And much of that marketing is dubious. Drug companies are not required to publish negative results of clinical trials conducted to obtain FDA approval. Such findings are considered proprietary, and though manufacturers must submit results of all clinical trials to the FDA, they are careful to publish only those showing effectiveness.
Moreover, the FDA requires only two clinical trials showing statistical difference between a drug and a placebo — or sugar pill — and drug companies can conduct as many trials as they wish. The statistical difference may even “be small enough to make no real difference in people’s lives.”
So says psychologist Irving Kirsch, Ph.D., of Harvard Medical School. In his book The Emperor’s New Drugs: Exploding the Antidepressant Myth, he published results of his 15-year-long investigation into the effectiveness of antidepressants. Using data directly from the FDA, he discovered placebos are three times as effective as no treatment and 75 percent as effective as antidepressants. The big difference between drug and placebo was that those taking the medication experienced negative side effects such as nausea, sexual dysfunction, and suicidal thoughts. Those on the placebo suffered no adverse effects.
But devious marketing does not stop there. Take the case of GlaxoSmithKline (GSK), which recently announced it will no longer pay doctors to promote its products. In January, best-selling author Dr. Joseph Mercola explained this seemingly altruistic announcement “was actually required as part of a corporate integrity agreement Glaxo made with the U.S. Justice Department.”
 He related that in 2012 GSK “plead guilty in the largest health fraud settlement in U.S. history.” The $3 billion suit involved illegal drug marketing of two antidepressants: Wellbutrin and Paxil. GSK had hired celebrities and a public relations firm to promote counterfeit claims about Wellbutrin. Mercola said, “One of the most high-profile accounts involved television celebrity Dr. Drew, who reportedly received $275,000 from GSK to promote Wellbutrin to treat sexual dysfunction associated with depression even though it hasn’t been proven effective for this purpose.”
He related that in 2012 GSK “plead guilty in the largest health fraud settlement in U.S. history.” The $3 billion suit involved illegal drug marketing of two antidepressants: Wellbutrin and Paxil. GSK had hired celebrities and a public relations firm to promote counterfeit claims about Wellbutrin. Mercola said, “One of the most high-profile accounts involved television celebrity Dr. Drew, who reportedly received $275,000 from GSK to promote Wellbutrin to treat sexual dysfunction associated with depression even though it hasn’t been proven effective for this purpose.”
More alarming still, GSK had manipulated Paxil clinical trial findings to downplay serious side effects in youth, using fraudulent information to market the drug for children and adolescents. Paxil is FDA-approved for adults only and bears the standard antidepressant black-box warning of suicide risk in young people. Unfortunately, this was not the first time GSK defrauded its Paxil consumers. The company paid fines of $2.5 million in 2004 for suppressing evidence that its top-seller “was ineffective and possibly harmful to children and adolescents,” wrote Marcia Angell, M.D., of Harvard Medical School. Angell is former editor-in-chief of the New England Journal of Medicine and an outspoken critic of the pharmaceutical industry.
GSK is not alone. Writing for The New York Review of Books in 2009, Angell lists Pfizer, TAP Pharmaceuticals, Merck, Eli Lilly, and Abbott among well-known offenders. In December 2013, the British Medical Journal (BMJ) published an article noting the “recent, sharp escalation in the frequency with which many giant multinational drug companies repeatedly engage in illegal criminal and civil activity after previously paying enormous fines” and despite ongoing monitoring. It accused these companies of incorporating unlawful behavior in their business models.
Conflicts of Interest
 Angell also exposes shocking collaborations between the healthcare community and big pharma, which help explain industry backlash to the FDA’s black-box warning. Drug companies routinely pay medical professionals as consultants and researchers, and they heavily subsidize professional organizations and medical education. They particularly target key opinion leaders at leading universities and institutions.
Angell also exposes shocking collaborations between the healthcare community and big pharma, which help explain industry backlash to the FDA’s black-box warning. Drug companies routinely pay medical professionals as consultants and researchers, and they heavily subsidize professional organizations and medical education. They particularly target key opinion leaders at leading universities and institutions.
For example, the chief of pediatric psychopharmacology at Harvard’s Massachusetts General Hospital, Dr. Joseph Biederman, is ranked as one of the world’s top key opinion leaders in psychiatry by the Institute for Scientific Information and is an influential advocate of diagnosing children as young as two with bipolar disorder. In 2008, investigations revealed Biederman accepted $1.6 million in consulting fees between 2000 and 2007 from drug companies, many of which manufacture the products he promotes to treat the condition. Most are not FDA-approved in children under 10. The hospital imposed a three-year probation on Biederman, limiting his access to “industry-sponsored outside activities.” Today, Biederman still occupies his eminent position in psychiatry.
Another case involves Dr. Alan Schatzberg, past president of the American Psychiatric Association and director of Stanford University’s Mood Disorders Center. He accepted National Institute of Mental Health (NIMH) grant money to research use of the abortion drug mifepristone (RU-486) in treating depression, while controlling more than $6 million worth of stock in a pharmaceutical company engaged in developing the drug for that use. Amid media buzz over this discovery, Schatzberg stepped down as principal investigator in the NIMH research but was reinstated soon afterward. [Also see Shrinks for Sale: Psychiatry’s Conflicted Alliance for other psychiatrists investigated for conflicts of interest.]
Congressional investigations in 2008 uncovered these and many other illicit ties between psychiatry and pharmaceuticals. One of the most scandalous involved Charles Nemeroff, past-chairman of Psychiatry and Behavioral Science at Atlanta’s Emory University School of Medicine. He resigned that position amidst investigations revealing he failed to disclose at least $1.2 million of the $2.8 million he earned from unethical alliances with drug and device manufacturers between 2000 and 2007. He now enjoys the prestigious position of chair of the Department of Psychiatry and Behavioral Sciences at the University of Miami.
Such conflicts of interest are now so prevalent the federal government has set up “Open Payments,” an online searchable database of financial relationships between drug companies and healthcare providers. It is part of the Affordable Care Act and answers Angell’s 2009 warning: “If the medical profession does not put an end to this corruption voluntarily, … the government … will step in and impose regulation. No one in medicine wants that.” But it’s doubtful Open Payments will protect the public from pharmaceutical wolves in doctors’ lab coats. The non-profit investigative news outfit ProPublica began a similar database in 2010 exposing the drug industry payroll. Though commendable, “Dollars for Docs” has done little to discourage fraud.
And it’s admittedly hard to trust a bureaucratic database when high-ranking government officials number among the guilty. The FDA incriminated itself on August 4, 2008, when it announced $50,000 to be the “maximum personal financial interest an [FDA] advisor may have in all companies that may be affected by a particular meeting.”
Congressional investigations in 2007 had exposed deeper conflicts of interest within the agency. Then-Congressman Bart Stupak (D-Mich.) testified that, prior to issuing its black-box warning, the FDA deliberately suppressed a wealth of research, including its own report, about antidepressant-induced suicidality in children. He said agency officials even “prohibited FDA employees from discussing the report and launched an investigation to find the person who leaked the information to the press.”
During that time Dr. Tom Laughren served as director of the FDA’s Division of Psychiatry Products (DPP) in the Center for Drug Evaluation and Research, where he held sway over approval and labeling decisions of all psychiatric drugs marketed in the United States and earned a controversial reputation for “close ongoing collaborative ties with pharmaceutical industry officials and industry-financed psychiatrists in academia and professional associations,” according to the Alliance for Human Research Protection. A longtime advocate of psychotropic drug use in children, he has often publicly dismissed related safety concerns, even those raised by FDA reviewers. Laughren retired from the agency in 2012 and now serves as director of regulatory affairs at the Massachusetts General Hospital Clinical Trials Network and Institute.
The Psychiatry Bible
 Devious marketing practices and industry corruption make headlines, but a more influential factor explaining the popularity of psychiatric drugs is the Diagnostic and Statistical Manual of Mental Disorders (DSM), the industry standard for diagnosing mental illness. Published by the American Psychiatric Association (APA) and currently in its fifth edition, DSM serves not only mental health professionals but also other physicians, social workers, therapists, insurance companies, and attorneys. The first edition, published in 1952, listed 106 mental disorders, and included homosexuality as a “sociopathic personality disturbance.” (Homosexual activists pressured the APA to remove it in 1974, underscoring criticism that cultural bias exercises ongoing influence over DSM.)
Devious marketing practices and industry corruption make headlines, but a more influential factor explaining the popularity of psychiatric drugs is the Diagnostic and Statistical Manual of Mental Disorders (DSM), the industry standard for diagnosing mental illness. Published by the American Psychiatric Association (APA) and currently in its fifth edition, DSM serves not only mental health professionals but also other physicians, social workers, therapists, insurance companies, and attorneys. The first edition, published in 1952, listed 106 mental disorders, and included homosexuality as a “sociopathic personality disturbance.” (Homosexual activists pressured the APA to remove it in 1974, underscoring criticism that cultural bias exercises ongoing influence over DSM.)
The current edition, DSM-V, published last year, dwarfs its original predecessor with 312 diagnoses, including hoarding, caffeine withdrawal, and Internet gaming disorder. Professor emeritus Allen Frances of Duke University, who chaired the manual’s fourth edition task force, wrote on his Huffington Post blog that the likely effect of the new 947-page tome will be “massive over-diagnosis and harmful over-medication,” especially because psychiatry is the only medical field with no objective tests, such as scans or laboratory findings, that justify diagnoses. “New diagnoses in psychiatry are more dangerous than new drugs because they influence whether or not millions of people are placed on drugs,” stated Frances, who noted primary care physicians write 80 percent of psychiatric drug prescriptions.
He said that during the manual’s latest revision process, the association turned a deaf ear to critics, including more than 50 mental health organizations that petitioned for an outside review. Small wonder. It seems DSM is more about profits than mental health. The Washington Post reports the drug industry has funded between 14 and 34 percent of the APA’s budget in recent years. At $199 a copy, DSM also pays a lot of the APA’s bills. Furthermore, the journal Psychotherapy and Psychosomatics reported in 2006 that some 56 percent of contributors to DSM’s previous edition had financial relationships with the pharmaceutical industry. There is little reason to believe the APA has reformed itself since, though Frances denies any impropriety. He attributes the explosion of mental health diagnoses to an “intellectual” conflict of interest “that results from the natural tendency of highly specialized experts to over value their pet ideas” in an eagerness to highlight their own areas of expertise.
Regardless, DSM’s broad diagnostic definitions ultimately aid drug manufacturers in creating demand for their products. In his 2007 book Shyness: How Normal Behavior Became a Sickness, Northwestern University professor Christopher Lane argues DSM turns relatively normal characteristics into diagnosable disorders, such as shyness, which is now labeled “social anxiety disorder.”
Moreover, diagnosing people with mental disorders teaches them to look for solutions in pills rather than in self-control. Excessive eating, once known as gluttony, is now a psychiatric illness known as “Binge Eating Disorder.” Behavioral Addictions introduced in DSM-V open the door to diagnosing mental illness for other types of extreme self-indulgence. “Disruptive Mood Dysregulation Disorder,” identified by Frances as one of DSM-V’s most potentially harmful additions, was referred to in former days as temper tantrums. He says it will likely result in a fourth fad in child psychiatry, adding to “a tripling of Attention Deficit Disorder, a more than 20-times increase in Autistic Disorder and a 40-times increase in childhood Bipolar Disorder” in the past two decades. It will also dissuade parents from properly disciplining their disruptive children while allowing them to be over-medicated with potentially harmful drugs.
The Long-term Cost
 Excessive diagnoses, over-medication, industry corruption, social stigmas, and moral decline are heavy fines the public now pays for easy access to psychiatric drugs. But research indicates long-term physical effects may present the hardest bill to pay. They stem from the action of psychotropics within the body’s central nervous system.
Excessive diagnoses, over-medication, industry corruption, social stigmas, and moral decline are heavy fines the public now pays for easy access to psychiatric drugs. But research indicates long-term physical effects may present the hardest bill to pay. They stem from the action of psychotropics within the body’s central nervous system.
Peter Gotzsche, medical researcher at Denmark’s Nordic Cochrane Centre, published an article in January explaining that, contrary to popular opinion, mental illness is not caused by imbalances of chemicals called neurotransmitters that allow brain cells to communicate. Study after study shows that, for example, people diagnosed with depression do not suffer from a serotonin deficiency, and schizophrenia patients do not have too much dopamine. However, introducing psychiatric drugs launches an artificial imbalance of these neurotransmitters, and the brain fights to stabilize the situation.
For instance, an antidepressant blocks removal of the neurotransmitter serotonin from the synapses between brain cells. The cells that secrete serotonin sense there is too much and release less of it, while the cells that receive serotonin become desensitized to it. This is a natural defense mechanism the body uses to achieve equilibrium. It is also the reason for the vast array of violent side effects that often accompany antidepressant use, especially when patients first start or stop taking the medicines. Serotonin affects many bodily functions such as mood, appetite, sleep, memory, and learning. An excess of it can cause potentially life-threatening symptoms, including mania, seizures, and rapid changes in heart rate and blood pressure.
Furthermore, when people stop taking antidepressants, the body needs time to readjust its compensatory mechanisms, setting the stage for additional severe reactions. In fact, discontinuation syndrome is such a problem that “weaning off the drugs can seem insurmountable, if not impossible, because of these negative side effects,” wrote Rebecca White in January for Al Jazeera, summing up her interview with psychiatrist and mental health expert Dr. Peter Breggin. “The result is an increasing number of Americans who have become married to their drugs to avoid the pain of getting off them.” Thus patients become dependent upon medicines originally intended only for short-term use.
Breggin, who has never prescribed a psychiatric drug in more than 40 years of successful private practice, employs broad-spectrum therapy involving psychosocial and educational approaches, as well as exercise regimens. Author of more than 20 books on mental health, he published a 2011 meta-analysis in the International Journal of Risk & Safety in Medicine of more than two dozen peer-reviewed reports that found long-term psychotropic use can lead to:
• Neuroleptic malignant syndrome, which causes brain cells to shrink and die and is nearly identical to viral encephalitis;
• Abnormal proliferation of neurons (brain cells), which induces “grossly abnormal” daughter cells;
• Tardive dyskinesia, a common disorder involving involuntary, repetitive body movements that is potentially disabling, usually irreversible, and known to lead to dementia;
• Generalized harm such as that associated with injuries from concussion, alcohol abuse, electroshock treatment, or other traumatic brain injury;
• Neuroleptic-induced deficit syndrome, which mimics schizophrenia; and
• General cognitive dysfunction and persistent biochemical changes.
Breggin says doctors often misdiagnose patients with early signs of these conditions, interpreting them as additional mental or physical illnesses instead of drug-induced reactions. Instead of safely weaning their patients off the offending meds, doctors add fuel to the fire with additional prescriptions.
But this is only a partial list, because psychotherapeutics affect the whole body, not just the central nervous system. They are associated with problems such as heart disease, respiratory illness, cancer, birth defects, and sudden death. People have ended up in court for bizarre behaviors committed under their influence, and defense lawyers are successfully using the drugs’ warning labels to mitigate or dismiss charges. The meds have formed an undeniable link with senseless acts of violence.
Such evils will continue to plague an over-medicated society fed on propaganda that life’s problems result from mental illness and that mental illness results from biochemical imbalances. Like alcohol and illegal drugs, psychiatric medications intoxicate the brain and wreak havoc on the body over time, yet society considers the former dissolute. The latter, with medical endorsement, are judged completely proper. The solution lies in people waking up to the dangers of psychotropic drugs and exercising educated judgment over their own healthcare and that of their children.
http://www.thenewamerican.com/usnews/health-care/item/17794-snared-by-drug-companies



SHARE YOUR STORY/COMMENT